Ozempic for Weight Loss: What You Need to Know and Why Nutrition Is Still the Gold Standard
Because your health journey deserves more than a quick fix.
Weight loss medications like Ozempic® (semaglutide) have taken the spotlight recently, thanks to celebrity endorsements and viral social media success stories. For many, the results look promising: reduced appetite, lower blood sugar levels, and dramatic weight loss. But is it as simple—and safe—as it looks? And what happens when you stop taking it?
Let’s explore the facts, side effects, and long-term implications of Ozempic and why a nutrition-based approach still remains the most sustainable way to lose and maintain weight.
What Is Ozempic?
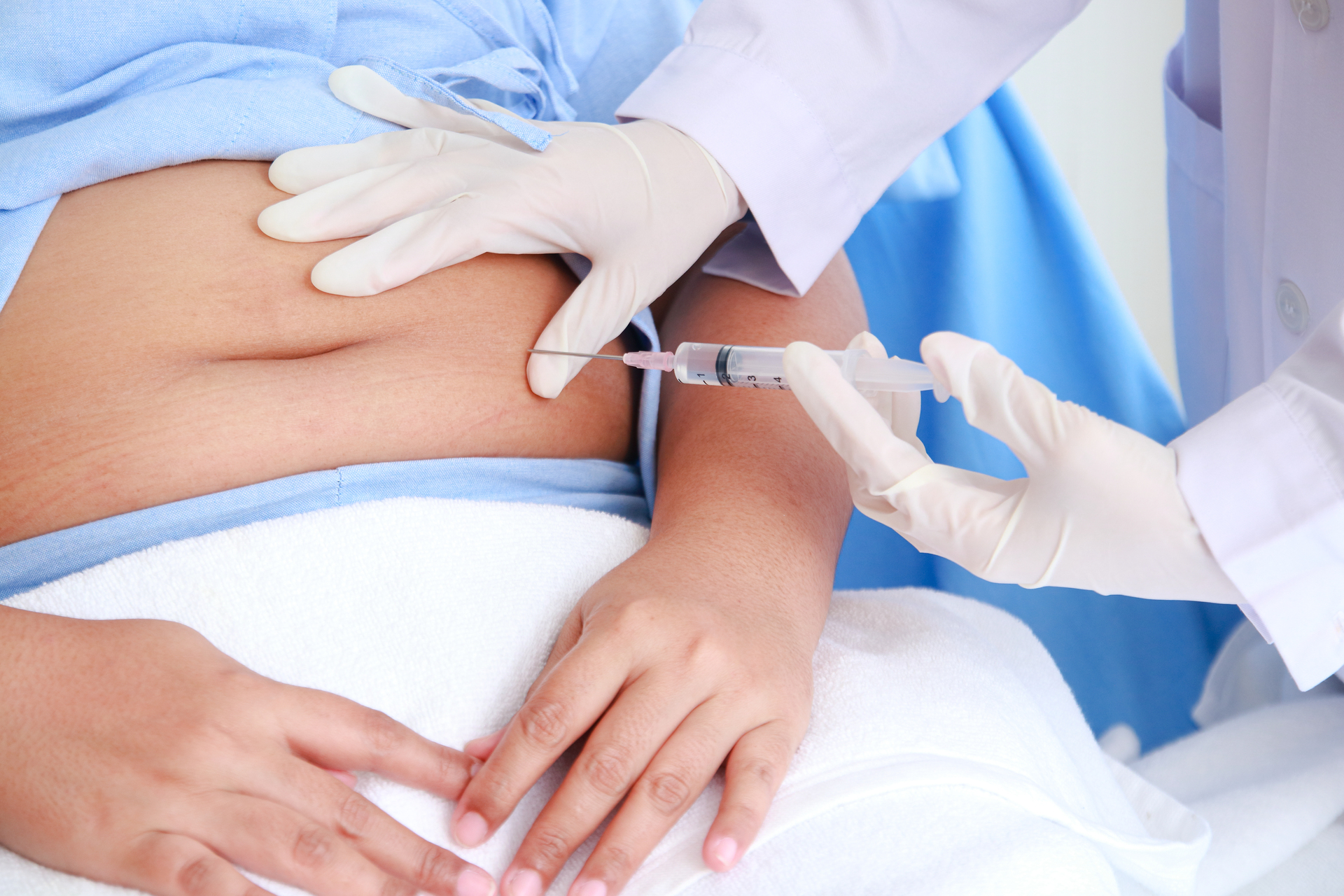
Ozempic is an injectable prescription medication originally designed to treat type 2 diabetes. It belongs to a class of drugs called GLP-1 receptor agonists, which:
Mimic a natural hormone that helps regulate blood sugar
Slow down digestion (delaying stomach emptying)
Reduce appetite and promote satiety
While Ozempic is FDA-approved for diabetes, it’s often prescribed “off-label” for weight loss.
How Does Ozempic Cause Weight Loss?
Reduced Appetite: You feel full faster and stay full longer.
Lower Food Intake: People often naturally reduce calorie consumption.
Improved Blood Sugar Control: Less insulin resistance can support fat metabolism.
Sounds like a miracle solution, right? But as with any medication, there’s more to the story.
Short-Term Side Effects
Many users experience mild to moderate side effects, especially during the first weeks:
Nausea, vomiting, or diarrhea
Constipation and stomach discomfort
Bloating or heartburn
Fatigue and dizziness
Headaches
These may lessen over time—but for some, they can be severe enough to stop treatment.
Serious & Long-Term Risks
Ozempic isn’t without serious potential health risks:
Pancreatitis: Inflammation of the pancreas, which can be life-threatening.
Gallbladder issues: Increased risk of gallstones and gallbladder disease.
Thyroid tumors: Shown in animal studies (human risk still being studied).
Muscle Loss: Rapid weight loss often includes lean muscle mass loss, lowering metabolic rate.
Rebound Weight Gain: When the medication is stopped, appetite often returns—and weight regain is common.
The Psychological Factor: Dependency & Body Image
Because Ozempic works by altering appetite and slowing digestion, many people worry about eating “normally” again. This can create:
Dependency on medication for weight control
Increased anxiety around food when stopping the drug
Potential for yo-yo dieting—a pattern proven to harm metabolic and mental health
The Nutrition Advantage: Why Food Is Still the Superior Medicine
Unlike medication, optimal nutrition and lifestyle changes:
Support metabolic health naturally (blood sugar, cholesterol, and hormones)
Build lean muscle, which increases calorie burn even at rest
Improve gut health, immunity, and energy
Reduce risk for chronic diseases without introducing medication risks
Empower you with lifelong habits—no injections, no dependency
Long-Term Weight Management: What Works Best?
. Balanced, Real Food Nutrition
Prioritize lean protein, fiber-rich vegetables, healthy fats, and whole carbs.
Avoid extreme restrictions and quick fixes—they often backfire.
2. Behavior Change
Focus on habits, not temporary diets (meal planning, mindful eating, stress management).
3. Muscle Mass Matters
Include strength training 2–3x/week to maintain and build lean muscle.
More muscle = higher metabolism and better long-term weight control.
4. Emotional & Mental Health
Address stress, depression, and anxiety, which can drive emotional eating.
Work with a coach or therapist for support, accountability, and confidence.
What About People Who Already Use Ozempic?
If you are using Ozempic under medical supervision:
Pair it with proper nutrition and exercise to preserve muscle mass.
Learn sustainable habits now—so if you stop the medication, you have tools to maintain your progress.
Regularly monitor labs and health markers with your healthcare provider.
The Bottom Line: Your Best Investment Is You
Ozempic may offer quick weight loss—but it comes with risks, unknowns, and dependency potential. Nutrition, strength training, and mindset work may take longer, but they give you:
A strong, healthy metabolism
A relationship with food you trust
Energy and confidence for life—not just while on a prescription
At Thrive Intensity, we focus on sustainable, evidence-based nutrition and lifestyle strategies so you can lose weight, improve health, and maintain results—naturally, safely, and for the long term.
Considering weight loss but want to avoid risky shortcuts?
Let’s create a custom nutrition plan that works with your body—not against it.
Click HERE to book your free consultation.













